Precision billing. Proven results. Less paperwork.


Why New Horizon Billing
Why New Horizon Billing
Specialized billing expertise
We understand the complexities of regenerative medicine and biologics, offering niche support where other services fall short.
Growth-focused support
Our solutions are designed to align with your business goals, support your practice, optimize performance, and promote sustainable, scalable growth.
Seamless integration with your existing systems
We connect with your current EHR and practice management platforms — streamlining workflows, reducing manual tasks, and ensuring a smooth transition.


Medical billing & claims management
We handle every aspect of claim submission — from coding and documentation to payer follow-up.

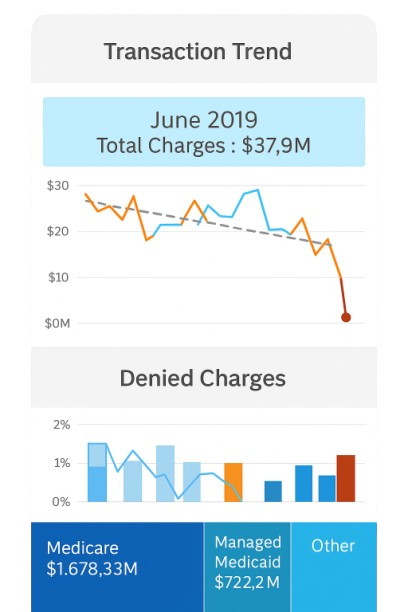
Revenue cycle management
Our end-to-end RCM services cover intake to reimbursement. We integrate seamlessly with your EHR and practice management systems.

Denial management
Denied claims don’t have to mean lost revenue. We proactively identify root causes, correct documentation gaps, and resubmit claims.

Accounts receivable management
We monitor aging reports, pursue outstanding balances, and optimize collection strategies.

Credentialing
We manage provider credentialing and payer enrollment from start to finish.

MIPS reporting
Stay compliant and maximize your Medicare incentives. We guide your practice through Merit-based Incentive Payment System (MIPS) reporting.

Practice optimization consulting
Beyond billing, we offer strategic consulting to improve operational efficiency. From workflow redesign to staff training and documentation protocols.

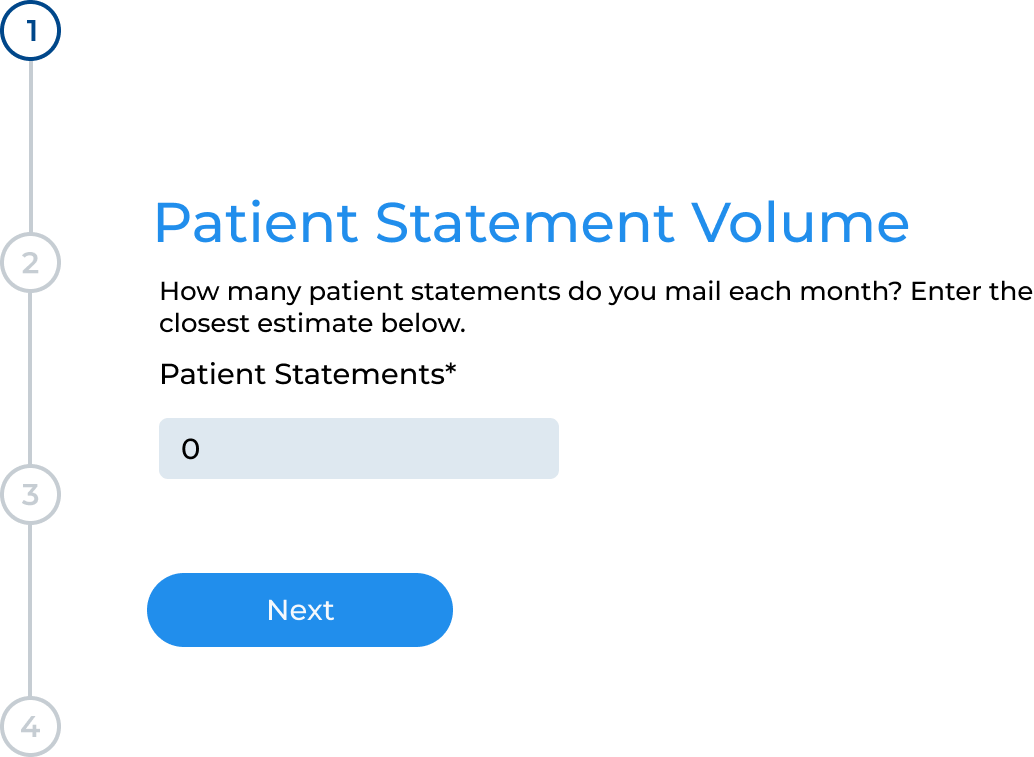
Calculate your annual savings
Trusted by

Ready to elevate your billing strategy?
Sitemap

Give us a call
1-725-271-1515

Send us an email
info@nhmbilling.com
